Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Use of Laser Therapy in Pressure Ulcer After Brain Vascular Accident
*Corresponding author: Clarissa Niero Moraes, Professor of the Physiotherapy Course, University of Southern Santa Catarina- UNISUL, Brazil.
Received: September 12, 2022; Published:October 13, 2022
DOI: 10.34297/AJBSR.2022.17.002331
Abstract
Pressure ulcers are a common factor in patients who are bedridden for a long time. There are preventive issues that can prevent their appearance, but when they arise it ends up being an inconvenience for the entire team. We report the case of a 53-year-old female patient who was treated with low-level laser electrotherapy. After four applications, the wound was completely closed. The low-power laser proved to be effective in the treatment and with fast action.
Keywords: Physical Therapy Modalities; Pressure Ulcer; Low-Level Light Therapy; Glucose; Oxygen; Brain Functions; Medical Monitoring
Introduction
The cerebrovascular accident (CVA) is characterized as a neurological hemodynamic dysfunction. Lesions are caused due to ischemia or heamorrhage, which results in impairment of brain functions [1]. It can occur in two ways: Ischemic CVA (CVAi) occurs when there is an obstruction in the vessel, preventing the delivery of glucose and oxygen, impairing the metabolic processes in the region. Haemorrhagic (CVAh) is less common, it is caused by an aneurysm or a rupture of an arterial brain wall [2]. In 2017, Brazil registered 101,100 deaths due to stroke. In 2018, 197,000 cases were registered in the Unified Health System (SUS) because of the pathology [3]. Risk factors increase the chances of a stroke, but most of them can be controlled with a change in lifestyle and medical monitoring. The main risk factors are high blood pressure, smoking, diabetes, sedentary lifestyle, obesity, high cholesterol, among other factors that can be considered risks [4]. When the CVA is not lethal, it causes functional and cognitive deficits depending on the location and extension of the lesion, making the patient dependent on hospital or home care. This lack of mobility can lead to the implication of pressure ulcers [5]. The appearance of pressure ulcers can occur due to increased pressure intensity, causing a deficiency in capillary perfusion, resulting in local ischemia. This situation is more recurrent in bony prominences that put pressure on the skin and soft tissues. The factors that contribute to the onset of the lesion are pressure, friction, moisture, immobility, altered sensitivity and advanced age [6]. The National Pressure Ulcer Advisory Panel 1 in 2007 [7], classified pressure ulcers as follows:
Stage 0:Suspected deep tissue lesion: localized purple or brown area, intact and pale skin, or blood blister due to soft tissue involvement by pressure and/or shear
Stage 1:Intact skin with hyperaemia maintained in an area located over a bony prominence
Stage 2:Loss of partial thickness of the dermis, seen as an ulcer with a red bed-pink, without necrosis, or blister with serous content
Stage 3:Loss of full thickness; subcutaneous can be visualized, but bones, tension and muscles not exposed
Stage 4:Full-thickness loss with exposed bone, tendon, or muscle; there may be necrosis
Not Classifiable:Full thickness loss, where the bed is-if covered by necrosis and/or eschar.
Physiotherapy aims to reduce the healing period in ulcerative processes, to facilitate the continuity of treatment without the patient feeling uncomfortable caused by the ulcer, enabling a faster return to their activities and an improvement in the quality of life of the patient and the caregiver [8]. The main objective of this study is to demonstrate the tissue repair process in pressure ulcers, through an equipment* composed of Laser (Light Amplification by Stimulated Emission of Radiation) and of Led (Light Emitting Diode) with red laser light emitting and blue LED light in a handle and infrared laser light and amber LED light [9]. Treatment through laser therapy improves the modulation of the inflammatory process, promoting healing and skin wounds, decreasing inflammatory cells, increasing fibroblast cells, and stimulating angiogenesis, formation of granulation tissue and increased collagen synthesis [8,9].
Methodology
This is a case study [10] carried out within the School of Physiotherapy Clinic of a local university, in Tubarão, Santa Catarina. The research subject is female, 53 years old with a diagnosis of CVA with sequelae of left hemiplegia, presenting a stage 3 pressure ulcer. The exclusion criteria used were pregnant woman, decompensated diabetes mellitus, immunosuppression, acute heamorrhage. According to the report of her caregiver, due to the use of alcohol, tobacco and blood pressure that was unregulated, the patient suffered the CVA, was found on the floor by her father, when she was rescued by the firefighters, she was still conscious, but confused. On January 26, 2021, he spent 30 days in the ICU where he developed a sore in the upper quadrant region of the left gluteus. Data collection was carried out through photos of the region, with iPhone 8 Plus® equipment, 12 Mega pixel rear camera, at 30cm in the Direction perpendicular.
Laser Photon Derm-DMC equipamentos
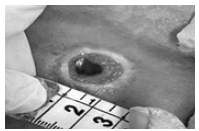
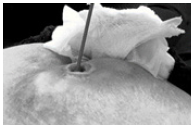
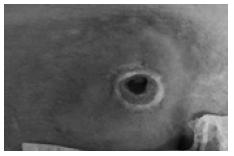
A manual measurement technique was used for width and length (Figure 1). The swab technique was also used to check the depth of the eschar, carefully inserting the swab into the wound (Figure 2). The instruments used to record the data collection were a visual analogue pain scale, an evaluation form containing information on the patient’s history and a photo of the lesion area. The research results were obtained through answers in the evaluation form and the visual analogue pain scale, informed by the patients in the first and last session of application of laser therapy, and the comparison between the photos of the first and last session. To supervise the evolution of the process, a record of the data that will be collected before and after each application session by photos will be used. For the application of the procedure, the Phto Derm® Laser equipment was used once a week, where the subject was in the prone position. The dressing was removed and applied to red light with a wavelength of 660nm±10 nm, selecting phototype III and IV, the applied dose was of intensity at 3J/cm², and applied in a spiral fashion (from inside the lesion to the outside), the average time was 4 to 10 minutes depending on the size of the ulcer [7] (Figure 3).
Results
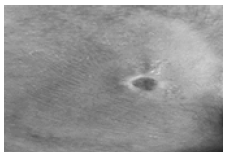
The pressure ulcer treated in this study achieved 100% healing after 4 applications of the Photon Derm@ laser, as shown in (Figures 4-6), in the second visit, an abrupt improvement of the pressure ulcer could be seen. in the 4th appointment, it was healed.
Discussion
Pressure ulcer, which can also be called decubitus ulcer, bed ulcer or eschar, is an aggravating condition for patients with little mobility, putting the patient at risk and complications. It is more frequent in public health institutions, requiring high cost in home and hospital treatment [11]. The incidence in neurological patients during the stay in intensive care units can reach 12.4% after a period of 6 to 4 days. In Brazil, the prevalence of pressure ulcers is 39.8% in patients at risk, admitted to university hospitals [6]. The prevention of pressure ulcers are relatively simple measures, one of them is the change of position in the bed, relieving the pressure on a bony prominence, it is important to avoid, during the change of position, that there are no movements that cause friction or shearing of the skin. Another example of prevention is to avoid humidity in the place, contact with urine, sweat or faces [6]. The physiotherapist plays a major role in preventing the development of pressure ulcers, by evaluating the integrity of the skin, offering measures to avoid the problem, using techniques to change position in bed, active or passive exercises and walking, favouring increased circulation blood leading to cellular nutrition. When the lesion is already present, the physiotherapist aims to contribute to and accelerate the healing process of pressure sores, using electrotherapy resources, such as other resources that help to increase the supply of nutrients [2].
Therapeutic laser has been related for more than 20 years, being initially applied in dermatology in the repair of skin wounds. According Lins et al. (2010) [12] Laser therapy, when used on tissues and cells, is not based on heating, that is, the energy of the absorbed photons is not transformed into heat, but into photochemical, photophysical and/or photobiological effects. Lowpower lasers have been used in tissue repair processes, as they have low energy density and wavelengths capable of penetrating tissues, demonstrating analgesic, anti-inflammatory and healing effects [12].
Conclusion
Despite being only a case study cannot fail to consider the satisfactory results found with the use of the Photo Derm® laser applied to red light with a wavelength of 660nm±10nm, selecting phototype III and IV, with dose of 3J/cm², and applied in a spiral (from inside the lesion to the outside), the average time was 4 to 10 minutes. In the bibliography a there are many controversies, and it is not possible to state which type of laser, which wavelength, or which dose is more suitable for the treatment of pressure sores. Thus, it is necessary to continue studies in this regard, with a larger number of patients, to verify whether the methodology proposed here is in fact statistically relevant.
References
- Leite D, Leite DF, Monteiro BBS, Matias LC, Sobral LL, et al. (2021) Physiotherapeutic care in a patient victim of aneurysm and hemorrhagic stroke: experience report. Mag CPAQV-CPAQV J 13(1).
- Facchinetti JB, Fernandes FP (2017) Resources used by Physiotherapists for Pressure Injury Prevention and Treatment. Psicol Mag. 11(37): 421-435.
- Ferezin SMR, Castro BM da C, Ferreira AA (2020) Epidemiology of transient ischemic attack in Brazil. Brazilian J Dev 6(8): 61125-61136.
- Cancela D (2008) Stroke-classification, main consequences, and rehabilitation.
- Damaceno G, Santos T, Rodrigues G. Use of photobiomodulation in the treatment of pressure injuries in stroke patients: literature review. Magazine Liberum accessum.
- Wada A, Neto NT, Ferreira MC (2010) Pressure ulcers. Med Mag 89(3-4): 170-177.
- (2021) National Pressure Injury Advisory Panel.
- Silvestre JT, Denise, Holsbach R. Physiotherapy performance in pressure ulcer: a review of literature.
- (2021) Photon Derm-DMC Equipamentos. Manualzz.
- Regina De AS, Ruoff AB, Piccoli T, Schmitt MD, Ferreira A, et al. (2017) Case study as a nursing research method: an integrative review. 26(4): 5360016.
- Stefanello TD, Hamerski CR (2006) Treatment of pressure ulcers using the 904nm EGaAs laser-A case report. Arch Health Sciences at UNIPAR 10(2).
- Diógenes R Lins AU, Dantas EM, Cristina K Lucena R, Maria HC Vasconcelos Catão, Ana Flávia Granville G, et al. (2010) Bio stimulation effects of low-power laser in the repair process. An Bras Dermatol: 85(6):849-55.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.